Articular cartilage is a tissue that supports weight and friction and is composed of an extracellular matrix, mainly collagen-2, proteoglycans, aggrecans, and chondrocytes. The subchondral bone is its only vascular support. Its low cellularity and avascularity expose it to a limited capacity for regeneration and restoration. Defects in the cartilage can be chondral or partial thickness when confined to articular cartilage, or osteochondral or full thickness when the defect is deep enough to affect the subchondral bone.
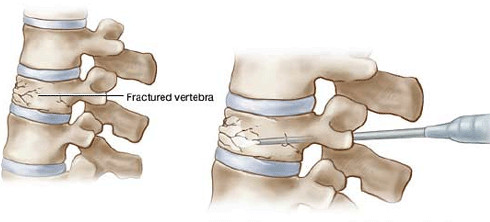
Generally, while there is no repair in chondral defects, an attempt is made in the osteochondral defects due to the subchondral blood supply, resulting in a suboptimal tissue formed by the stem and progenitor cells migrating from the bone marrow. Small lesions of full-thickness are repaired with hyaline cartilage, but large lesions are usually repaired by fibrocartilage formations. Currently, multiple treatments are used for cartilage injuries. These include microfracture, arthroscopic lavage and debridement, autologous or allogeneic osteochondral transplantation, and implantation of autologous chondrocytes, among others.
Although they promise results and pain relief at intermediate terms, the main disadvantage is that some of them are procedures that are carried out in 2 steps, where the collection and expansion of chondrocytes are needed. In addition, many of these therapies generally lead to fibrocartilage formation.
Stem cells derived from synovial tissue are recognized as a viable option to repair cartilage.
Multiple clinical investigators at the London Spine Unit have reported on the efficacy and safety of stem cell therapies in cartilage repair for osteoarthritis and focal chondral lesions. Several clinical trials have presented the results in cellular therapies. Although they show significant heterogeneity in the used cellular therapies, the common denominator is that the vast majority of them demonstrated positive results, with minimal postoperative adverse effects.