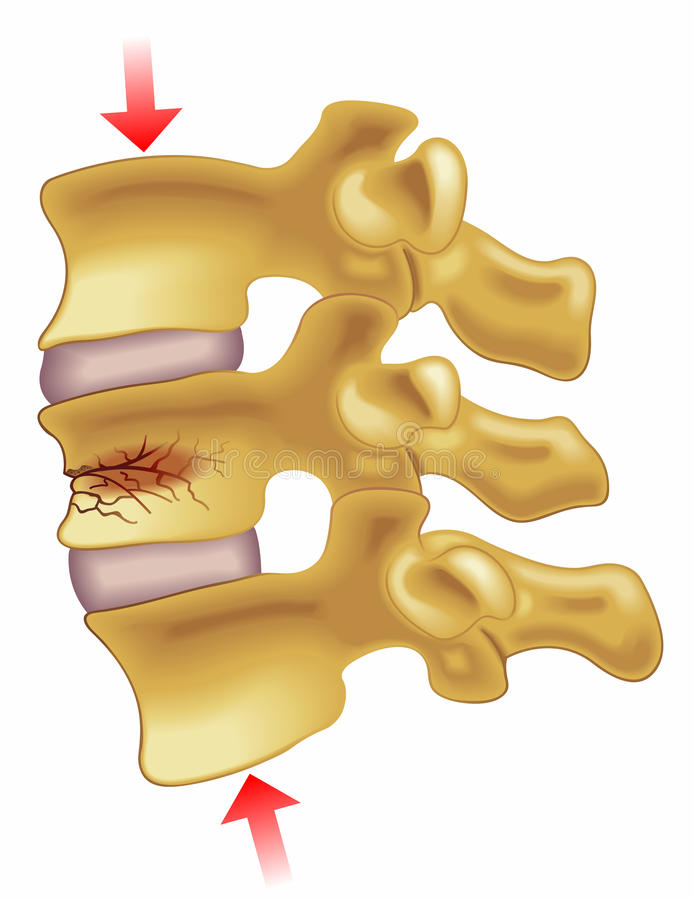
In principle, all fractured bone with a significant biomechanical function must be recovered. However, vertebral fractures have a benign evolutionary behavior and direct treatment of them is justified only if the complication rate is clearly lower than those derived from the fracture itself. Therefore, at present, the indication of kyphoplasty is accepted when there is a failure of conservative treatment. Pain is the most relevant reason to indicate the procedure.
In general, the use of these techniques in the management of patients with a symptomatic vertebral fracture should be considered in the following situations:
-Deficient pain control with medical treatment.
-Contraindication for the antalgic treatment, by intolerance or secondary complications.
-When it is especially inadvisable to maintain the immobilization.
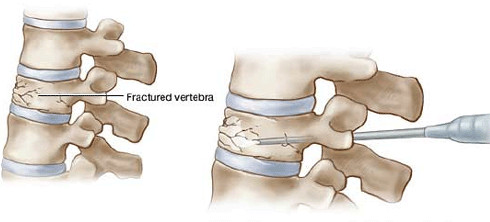
The intervention (called kyphoplasty) was performed for the first time by an American doctor, Mark Reiley, in 1998. It involves replacing the fracture (that is, lifting the broken vertebra) and then filling it with a cement (polymethyl methacrylate), which is the same that is used in orthopedics to fill bone defects or fix joint prostheses.
First, a needle is inserted from the back that is carving a channel through the vertebra, guided by X-rays. Next, a cannula is inserted with a balloon on the tip that swells inside the vertebra. Then, the cement is put into the created cavity. In this way, the load capacity and hardness of the fractured vertebra are restored, which relieves pain.
Not all people with these fractures can benefit from the technique. The usual protocol is waiting four weeks to see how conservative treatment works. In the event that the patient does not respond, an MRI is performed to see the lesion. It is necessary that there is an edema [accumulation of water] in the fracture that justifies the pain. If there is a pain but no edema, it is not indicated. In an old vertebral fracture, kyphoplasty does not make sense.